A century on from our first polio epidemic and 50 years after our last, many New Zealanders still live with the after-effects of the disease. Finding appropriate and timely services and support is as hard for them as any other impairment group.
However, they tend to be older and more stoic than the younger generation of disability advocates and their needs and stories are often overlooked. We don’t know how many New Zealand survivors are left, but many of us have family and friends who are affected.
From the first epidemic in 1916 until the last in 1961, polio was a feared disease, as it mainly affected children and young adults. Initially known as Infantile Paralysis, it struck randomly, had no cure and peaked in regular epidemics. There were about 10,000 reported cases in NZ over 50 years.
But by 1960 both the Salk and Sabin vaccines were available in New Zealand and new cases diminished apart from those infected overseas. Many years after their original infection, survivors started reporting new symptoms and in the 1980s the condition of Post-Polio Syndrome was identified. Internationally, the battle to eliminate polio continues, with fewer than 40 new cases reported so far this year.
‘Poliomyelitis’ means grey marrow and ‘itis’, inflammation – so the condition more commonly known as polio is an inflammation of the spinal cord, or central nervous system. Polio is a highly contagious viral illness which enters by the mouth or nose then travels down into the gut.
There are three types of poliovirus. The virus spreads from the gut into the blood and lymph system to the spinal cord. It attacks nerve cells or motor neurons in the spinal cord, disrupting their pathways, although other neurons can sometimes take over and form new pathways. The virus is present in the faeces of an infected person so can be spread by hurried hygiene, or via infected mucus.
The incubation time in the body is usually about one to two weeks. Symptoms can include digestive upset, fever, stiff neck, muscle and nerve pain, and sensitivity to light (similar to meningitis). It often manifests as a mild cold, or flu like symptoms, for several days following which muscles suddenly become extremely painful and fever intensifies. Commonly affected are the arms, legs and lower body; most serious is bulbar polio which damages muscles around the diaphragm, lungs and throat, threatening breathing and swallowing.
More than 90% of people infected have mild or no symptoms while others experience temporary pain and paralysis. Fewer than 1% of those exposed to the virus are permanently impaired. So it can be widespread in the population but only a tiny proportion of those infected will be left paralysed.
Polio paralysis is different from spinal cord injury as the feet and hands still have feeling, such as feeling the prick of a pin. Some neurons and muscles can regrow if not too badly damaged. Immobilisation of the affected limb is thought to encourage muscular atrophy (withering) while massage and physiotherapy may help muscle cells regrow.
There is evidence that polio has been around for centuries. But the first reported cases in New Zealand were in 1880 and the first recorded cases in 1914 in the Otago Southland area, and that outbreak led to polio becoming a notifiable disease.
Polio provides a canvas for evolving theories of epidemiology and interventions. One theory for why it started to increase in the early years of the 20th century with the first big epidemic internationally in 1916 is that as hygiene improved and diseases like diphtheria and dysentery decreased, polio took hold.
It was assumed to affect only children, because some believed that the germs which caused the condition lived close to the ground and thus only infected small people. However, natural community immunity probably meant at first only children were affected. By the mid-20th century more young adults were becoming victims.
Polio scared families and communities, as it struck apparently randomly and crossed class lines. It caused considerable stigma for affected families. Schools were often closed for several weeks and families confined to their disinfected homes to prevent further contamination.
While many infected children and adults were sent to one of the many polio hospitals across New Zealand, often for months at a time, others were treated by GPs or small local hospitals, where knowledge about polio varied. Survivors commonly recall being sent away from family for weeks or even years for hospital treatment and rehabilitation.
Although there were New Zealand polio cases intermittently through the years several epidemics of over a thousand reported cases each happened in 1916, 1925, 1936-7, 1943, 1947-8, 1953 and 1955-6. 1961 was the last and the smallest. It is likely that over the years cases were underreported, with suggestions that only about 20% were actually notified. More than 800 New Zealanders died from polio between 1916 and 1961. Epidemics peaked over summer and some survivors remember a pool swim as their point of infection.
By the 1930s, standard treatment was immobilisation of the affected limb initially with plaster, often for long periods. A calliper (also known as irons), consisting of a metal plate under the foot laced up around the leg, provided permanent support.
Elizabeth Kenny, an Australian nurse who served on transport ships in WW1, developed an innovative treatment. She pioneered work in muscle rehabilitation using regular application of sharply contrasting temperatures, and massage. After she moved to the US in 1940 her treatment became widely used. Her advocacy of massage and opposition to long term immobilisation became the basis of the new science of physiotherapy.
For those unfortunate enough to have impaired breathing as a result of the polio infection mechanical help was required. Treatment consisted of lying in a negative pressure ventilator known as an iron lung – a coffin-like structure enclosing the whole body apart from the head – which stimulated the breathing reflex. The patient might stay in that box for weeks or even years. There was a high mortality rate for those affected, as pneumonia was a constant risk in the days before routine administration of antibiotics.
Philanthropy has played an important role with polio over the decades. During the Depression it was particularly tough for many families struggling to support their affected child.
Orthopaedic surgeons, frustrated at the lack of services for polio victims who couldn’t afford hospital care, therapy or aids, started lobbying. Surgeon Dr Alexander Gillies spoke to the Wellington Rotary Club as early as 1930 about the needs of the estimated 5000 ‘crippled’ children in New Zealand – those with polio and other conditions such as spina bifida. In 1935 Dr Gillies and Charles Norwood of the Wellington Rotary Club launched the New Zealand Crippled Children Society.
The CCS was gifted a large home in Takapuna, Auckland, and major donations, including £10,000 from Mr and Mr Wilson. The Wilson Home became a hospital for physically disabled children, including those with polio.
With help from Rotary, CCS branches were set up around the country to provide home support, travelling clinics, advice and aids and appliances. War experience provided valuable training to orthopaedic surgeons such as Dunedin’s Major Renfrew White, who brought his Second World War experience of fixing up injured servicemen into civilian work with polio.
In the mid-1940s another philanthropically-minded landowning couple, Thomas and Jeannie Duncan, established a trust to treat polio. They founded a polio hospital in Silverstream near Wellington, later relocating to Wanganui. The Trust paid for several health professionals to go to the United States for training in the Kenny technique.
Elizabeth Kenny’s nephew Bill Bell, later helped by his son, worked at the Wanganui hospital until its closure in 1979. Children and adults from across New Zealand attended the hospital for treatment and lived there for months or years, or returned regularly. The therapy consisted of daily intensive heat pack treatment, followed by long and sometimes painful physiotherapy sessions to stretch and strengthen muscles.
The arrival in New Zealand of the first vaccine in 1958 was a major event and few people here have contracted polio since 1961. But years after their initial infection, many adult survivors experienced new symptoms of pain, fatigue, muscle weakness and atrophy. One theory was that the nerve ends or motor neurons which grew extra ‘sprouts’ to compensate for the earlier damaged ones have a limited life. This condition is known as post-polio syndrome.
The vaccine story
The polio vaccine story is fascinating. President Roosevelt was apparently a polio survivor. He was 39 when he became paralysed in 1921, presumably by polio, although he was older than most victims. Paralysis permanently affected both his legs but his impairment was hidden from the public and for each public appearance there was an elaborate effort to prop him upright with heavy metal callipers.

One of only three known photos of Roosevelt in a wheelchair. Here with girl wearing a leg calliper. (Wikpedia)
Roosevelt’s interest in polio was widely known and before he became president he established a rehabilitation centre in Georgia. It apparently had a ‘whites only’ admission policy on the assumption that polio only infected white people.
In 1938 he established a foundation to fight polio. A well-known entertainer suggested people donate dimes (10 cent pieces), and the foundation then known as the March of the Dimes provided funding and advocacy for a vaccine. Meanwhile, it seemed black people could indeed catch polio and in 1941 a polio research centre was opened in the black university at Tuskagee, Alabama, to train black doctors and physiotherapists.
Early researchers attempted to develop a killed vaccine from monkey spinal cords. But the first person to conduct a human trial for an attenuated oral polio virus (OPV) was Polish born American immunologist, Hilary Koprowksi, in 1950. An attenuated virus is a live virus diluted to safe enough levels to cause an immune response, but not illness, in humans. Animals are often used for the attenuation process ‒ in this case rats, later monkeys.
After first taking it himself, Koprowski tested his attenuated Type II (one of the three strains) OPV on one child in a New York state institution for children with intellectual disability. When that child seemed OK, he tried it on 19 more. The practice of testing drugs and other experimental interventions on institutionalised disabled children and adults was common. Some thought the testing, particularly of a live virus, premature. Fortunately, none of the children became ill and all developed Type II antibodies.
Then the prolific HeLa cells became available. Henrietta Lacks was a black woman who died of cervical cancer in 1951. Her HeLa cancer cells had the rare property of reproduction in the laboratory and became the basis of modern medical research, including polio. Science writer Rebecca Skloot’s story The Immortal Life of Henrietta Lacks, of how Henrietta’s cells were exploited without thought to ethical principles or any compensation for her family, is one of our modern treatises on the intersection of clinical research, ethics, race and gender. But in 1951, the rush was on for a cure for polio.
Koprowski’s live virus proved difficult to prepare in the quantities required. Jonas Salk, a US virologist, instead developed vaccine from the HeLa cells for all three polio strains from the dead virus which could be injected. He then found some captive intellectually disabled children in institutions on whom to test his vaccines in various combinations, and found they produced relevant antibodies. A massive trial then immunised more than a million US children in 1954, and the vaccine was licensed in 1955. In a magnanimous gesture, Salk never patented the vaccine. Immunisation via the IPV (inactivated polio vaccine) injection came to NZ in 1958 with much publicity.
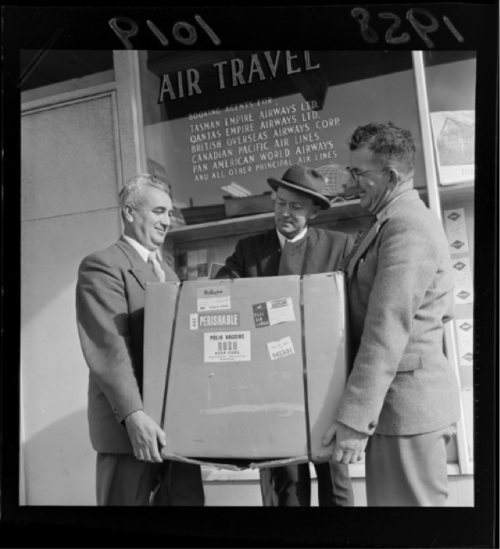
Three men holding a carton of Polio Vaccine, standing outside the Tasman Empire Airways Ltd office. 1958 Evening Post newspaper. Ref: EP/1958/1019-F. Alexander Turnbull Library, Wellington, New Zealand.
Meanwhile, another Polish-American medical researcher, Albert Sabin, adapted Koprowski’s live virus to develop vaccines for all three polio strains. He had spent years attenuating the polioviruses so that they would induce immunity but not be iatrogenic, meaning the vaccine would not itself cause disease.
Sabin worked with Soviet health officials who were interested in a cheaper alternative to Salk’s vaccine. His OPV was given to 10 million Soviet children in the mid-1950s. It had several advantages over the Salk vaccine: it was delivered orally so did not require an injection; it went through the digestive system in the same way as the virus, and human excrement containing vaccine remnants helped create weak immunity in the community. A risk was that the live virus could also revert to the virulent form.
The US Surgeon General recommended licensing of Albert Sabin’s live Type I poliovirus vaccine in 1961. Vaccines for Types 2 and 3 followed and a 1963 vaccine combined all three. Vaccination against polio is now part of the immunisation schedule for all New Zealand babies, as it is in most countries.
Despite the availability of a safe vaccine for more than 50 years, the story of polio infection unfortunately continues. Rotary International took on the cause in 1979 with its End Polio Now campaign. They named 24 October as World Polio Day to commemorate Salk’s birthday in 1914. The Bill and Melinda Gates Foundation also funds campaigns.
By 2011, polio was almost eradicated globally with only three countries still reporting cases: Pakistan, Afghanistan and Nigeria. However, politics intervened. That year, the CIA used a hepatitis vaccination programme as cover to help locate and kill Al Qaeda leader Osama bin Laden in Pakistan. Several polio vaccinators – many of whom were women earning precious money by giving out drops – as well as security personnel, were then attacked and killed. Rumours abounded that the vaccine contained pork or was a plot to sterilise Muslims. The Taliban banned vaccination in their area of Pakistan near the Afghan border.
So in 2014, polio was spreading again in Africa and Middle Eastern conflict zones. Many of the new infections in Syria were young children who had missed their immunisations due to the war.
In April 2014, the World Health Organisation met to consider how to contain the spread of endemic poliovirus (already present in the population) and wild poliovirus (usually spread by adult travellers). The WHO declared the spread a Public Health Emergency of International Concern. Such warnings are very rare but it appeared to be effective and the last resistant area is the region around the Afghanistan-Pakistan border. In May 2015 the World Health Assembly adopted a resolution to finish polio once and for all. Only 34 new cases have been reported this year – 28 in Pakistan and six in Afghanistan. But there is still risk, particularly in conflict or disaster zones, as one case can mean 200 people are infected.
The polio story is not over yet.